Rabies prevention
Because of the high fatality rate, the prevention of rabies infection is of utmost importance.
Please visit the WHO site for the latest recommendations on rabies prophylaxis
WHO guide for rabies prophylaxis
WHO strongly recommends discontinuation of the nerve tissue vaccine, and replacement with modern concentrated and purified cell culture derived vaccines (CCDV) and embryonated eggbased rabies vaccines. These vaccines must comply with WHO criteria for potency and innocuity following satisfactory assessment in humans during well-designed field trials.
Pre-exposure prophylaxis
Generally, pre-exposure vaccination should is recommended to anyone at continual, frequent or increased risk for exposure to the rabies virus such as those working in rabies diagnostic or research laboratories, veterinarians, animal handlers (including bat handlers), animal rehabilitators and wildlife officers, as well as other people (especially children) living in or travelling to high-risk areas.
Post-exposure treatment
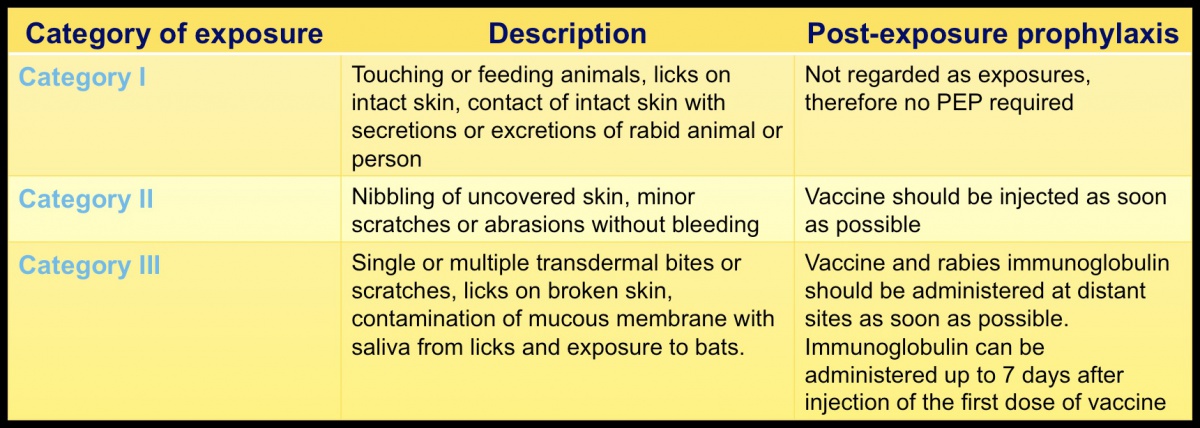
After exposure, prevention of infection is virtually assured by post-exposure prophylaxis consisting of local treatment of the wound (see below), initiated as soon as possible after an exposure, followed by the administration of a potent and effective rabies vaccine that meets WHO criteria and a passive immunization, if indicated (category III). A risk assessment conducted by a medical expert knowledgeable in the epidemiology of rabies in the area should be performed. Depending on adequate laboratory surveillance authorities may not recommend post-exposure prophylaxis.
Local treatment of wounds
Any bite wound or scratches that might be contaminated with rabies virus should immediately be flushed with rinsing water as first-aid procedure! Thorough washing for a minimum of 15 minutes with soap and water, detergent, povidone iodine or other substances of proven lethal effect on rabies virus or other detergents should follow. This will drastically reduce infectivity of the virus. Suturing of the wound should be avoided. Bleeding at any wound site indicates potentially severe exposure and must be infiltrated with either human or equine rabies immunoglobulin. Other treatments following bite inflictions should include administration of antibiotics and tetanus prophylaxis.
In countries or areas enzootic for rabies, exposure to suspected or confirmed rabid animals are categorised by WHO as follows:
For detailed information on vaccination regimens ask your national health authorities or see WHO-pages on rabies: www.who.int/rabies
Still the best possible way to prevent rabies is to keep away from rabies suspect animals
(see clinical signs).